Key Points:
- Self-care must be integrated into counselling curricula and supervision practices.
- Reflective practices and regular wellness check-ins build self-awareness.
- Peer support networks help reduce isolation and stress.
- Institutional policies must actively support trainee mental health.
- Teaching adaptive coping skills prepares trainees for sustainable practice.
In the evolving landscape of mental health education, the importance of self-care is universally acknowledged. Yet acknowledgment alone is insufficient. Without practical, deliberate strategies to embed self-care into training and practicum supervision, good intentions quickly dissipate.
This fourth article of our five-part series moves beyond theory to explore concrete, evidence-based strategies that programs, supervisors, and trainees can use to ensure that self-care becomes a professional norm, not a forgotten aspiration.
Why Action Matters
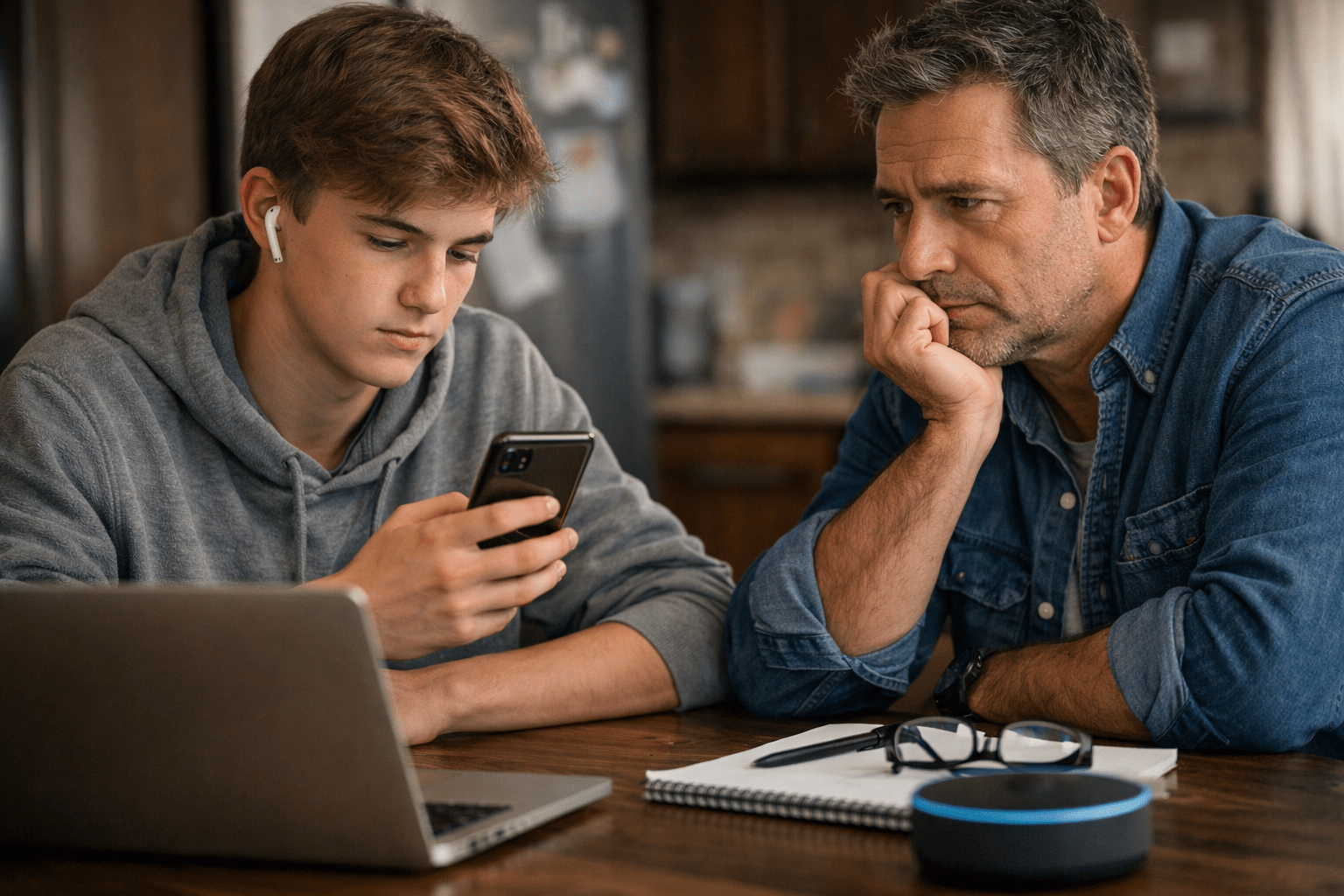
Counselling students face a paradox: while taught to advocate for their clients’ wellness, they often receive little structured support for their own.
Embedding self-care into the training process must be intentional, systematic, and evaluated (Grise-Owens et al., 2018).
Trainees thrive when self-care is treated with the same seriousness as clinical skills acquisition—through curriculum integration, reflective practice, structured supervision, and supportive policies (Myers et al., 2022).
Without deliberate action, the risks are too great: burnout, ethical impairment, compassion fatigue, and ultimately, compromised client care.
Strategy 1: Make Self-Care a Core Curriculum Component
The first step is simple but radical: treat self-care as a core competency.
Courses on ethics, clinical skills, and multicultural competence are staples in counselling programs. Self-care should have a similar standing.
This can include:
- Stand-alone courses on wellness strategies.
- Integrating self-care topics into existing courses.
- Mandatory self-care planning assignments.
Callan et al. (2021) emphasized that structured self-care training during graduate programs significantly enhances resilience and prevents early career burnout.
Practical Tip:
Assign students to create, present, and revise personal self-care plans each semester, aligning with developmental and practicum milestones.
Strategy 2: Incorporate Reflective Practices
Reflection bridges awareness and behaviour.
Reflective practices such as journaling, supervision discussions, mindfulness, and group processing help students internalize the emotional demands of the work and foster deeper self-awareness (Curry & Epley, 2022).
Supervisors and educators can:
- Build reflection into supervision contracts.
- Assign weekly or biweekly reflective journals focusing on emotional self-monitoring.
- Facilitate group discussions about emotional responses to client work.
Practical Tip:
Encourage trainees to reflect not only on client issues but on how their own emotions and experiences intersect with their professional development.
Strategy 3: Normalize Conversations About Wellness
A persistent barrier to self-care is stigma: the belief that needing rest or support signals weakness.
To dismantle this, wellness must become part of the regular dialogue in classrooms, supervision, and practicum sites (David & Achempim-Ansong, 2021).
Supervisors can model vulnerability by sharing their own self-care struggles and successes. Faculty can open discussions about mental health challenges during training, normalizing that seeking support is responsible, not shameful.
Practical Tip:
Open each supervision or practicum class with a “self-care check-in” alongside clinical updates.
Strategy 4: Build Peer Support Networks
Isolation is a major contributor to stress in graduate training.
Peer support acts as both a protective factor and an accountability structure.
Programs can foster this by:
- Organizing wellness or support groups.
- Encouraging peer mentoring between senior and junior students.
- Creating informal spaces (online or in-person) for self-care discussions.
Mills et al. (2018) found that peer-based approaches significantly reduce feelings of stress and helplessness among health care trainees.
Practical Tip:
Designate a “wellness representative” in each cohort responsible for organizing periodic group self-care activities.
Strategy 5: Develop and Implement Institutional Policies that Support Wellness
Beyond individual and interpersonal strategies, systemic change is crucial.
Institutions must critically examine how their policies either promote or hinder self-care (Myers et al., 2022).
Supportive policies might include:
- Reasonable limits on practicum hours.
- Mandated breaks or mental health days.
- Access to free or low-cost counselling services for trainees.
- Clear protocols for addressing trainee impairment.
When wellness is backed by policy, trainees are more likely to prioritize it without fear of academic or professional penalty.
Practical Tip:
Include self-care expectations and supports explicitly in practicum handbooks and training contracts.
Strategy 6: Teach Adaptive Coping and Resilience Skills
Simply advising students to “practice self-care” is not enough.
Programs must teach concrete coping strategies such as:
- Mindfulness and meditation techniques (Choi & Hyun, 2023).
- Stress inoculation training.
- Cognitive-behavioural coping skills.
- Boundary-setting exercises.
Guler and Ceyhan (2021) demonstrated that explicit self-care training improves resilience and perceived self-efficacy in counselling students.
Practical Tip:
Host workshops on topics like “Saying No Effectively” or “Managing Compassion Fatigue” as part of practicum preparation.
Strategy 7: Evaluate Self-Care as Part of Professional Competence
What gets measured, gets prioritized.
If self-care is truly a professional skill, it should be assessed alongside clinical competencies.
Evaluation could include:
- Self-care plans and their updates.
- Reflective papers on wellness practices.
- Supervisor evaluations of boundary maintenance and self-awareness.
Evaluating self-care sends a clear message: wellness is integral to being an effective therapist.
Practical Tip:
Use formative assessments that give students feedback on their self-care progress rather than punitive grades.
A New Paradigm for Training
Embedding self-care into training is not an extra task.
It is a cultural shift that recognizes the humanity of therapists-in-training.
When programs teach self-care systematically, model it authentically, and support it institutionally, they produce graduates who are:
- More resilient,
- More ethical,
- More effective.
The old model—survive graduate school at any cost and patch yourself together later—must be replaced with a new vision where wellness and professional development grow hand-in-hand.
As educators, supervisors, and institutions, we must build systems that protect, not just produce, the next generation of therapists.
About the Author
Father Pishoy Wafsy
Rev. Fr. Dr. Pishoy Wasfy, PhD, MDiv, RP, is an ordained Coptic Orthodox priest serving in Mississauga, Ontario, and a Registered Psychotherapist with over 14 years of counselling experience. He holds a Ph.D. in Christian Counselling, a Master of Divinity in Clinical Counselling, and a Bachelor of Science in Pharmacy from the University of Toronto. Fr. Pishoy integrates clinical expertise with spiritual care, supporting individuals, couples, and families through his work at Cornerstone Family Counselling Services and broader community initiatives.

References
Callan, J. E., Smith, C. M., & Meiser, D. (2021). Self-care training methods in counselor education: A systematic review. Teaching and Supervision in Counseling, 3(1), 1–18. https://doi.org/10.7290/tsc030101
Choi, Y., & Hyun, M. (2023). The role of mindfulness-based self-care in counselor education: Enhancing resilience and reducing stress. Journal of Counselor Preparation and Supervision, 16(1), Article 6. https://doi.org/10.7729/16.1.6
Curry, J. R., & Epley, L. E. (2022). Reflective practice as self-care in counselor education and supervision. Journal of Counselor Leadership and Advocacy, 9(2), 143–157. https://doi.org/10.1080/2326716X.2022.2048991
David, S., & Achempim-Ansong, R. (2021). Student counsellor self-care: Conceptual and practical considerations. Journal of Counselling Practice, 8(1), 1–13.
Grise-Owens, E., Miller, J. J., & Eaves, M. (2018). Teaching note—Advancing self-care in social work education: Reflections on a pedagogical framework. Journal of Social Work Education, 54(1), 187–194. https://doi.org/10.1080/10437797.2017.1302857
Guler, D., & Ceyhan, E. (2021). Self-care training for counselor trainees: The effect on self-efficacy and resilience. European Journal of Psychology of Education, 36(2), 417–437. https://doi.org/10.1007/s10212-020-00483-1
Mills, J., Wand, T., & Fraser, J. A. (2018). Exploring the meaning and practice of self-care among palliative care nurses and doctors: A qualitative study. BMC Palliative Care, 17(1), 63. https://doi.org/10.1186/s12904-018-0318-0
Myers, S. B., Sweeney, A. C., Popick, V., & Wesley, K. (2022). Institutional barriers and supports for graduate student wellness: Perspectives from faculty and students. Training and Education in Professional Psychology, 16(2), 147–155. https://doi.org/10.1037/tep0000351