TLDR: Quick Guide for Parents
When to be concerned: Watch for changes that last weeks, not days. Trust your gut if something feels off.
Common signs: Sleep/eating changes, persistent irritability, social withdrawal, sudden friend group shifts, dropping grades, physical complaints without medical cause, expressions of hopelessness.
What’s normal: Mood swings, wanting privacy, some conflict, friendship drama, testing boundaries.
Mental health is common: Nearly half of all adolescents will experience a mental disorder during their teen years. Seeking support is healthcare, not weakness.
How to talk about it: Keep it simple. Emphasize privacy and normalize therapy. Don’t make it sound like punishment or “fixing” them.
Crisis vs. ongoing support: If your child shares thoughts of self-harm or suicide, seek professional help immediately. You can contact a crisis line such as 988 for guidance, and call 911 if you’re concerned about their immediate safety. Ongoing therapy can help children develop skills to cope with suicidal thoughts, self-harm urges, and other underlying struggles.
Next step: Book a free 15-minute consultation with Nada, Karoline or Lauren or call us at 905.214.7363 to discuss your concerns.
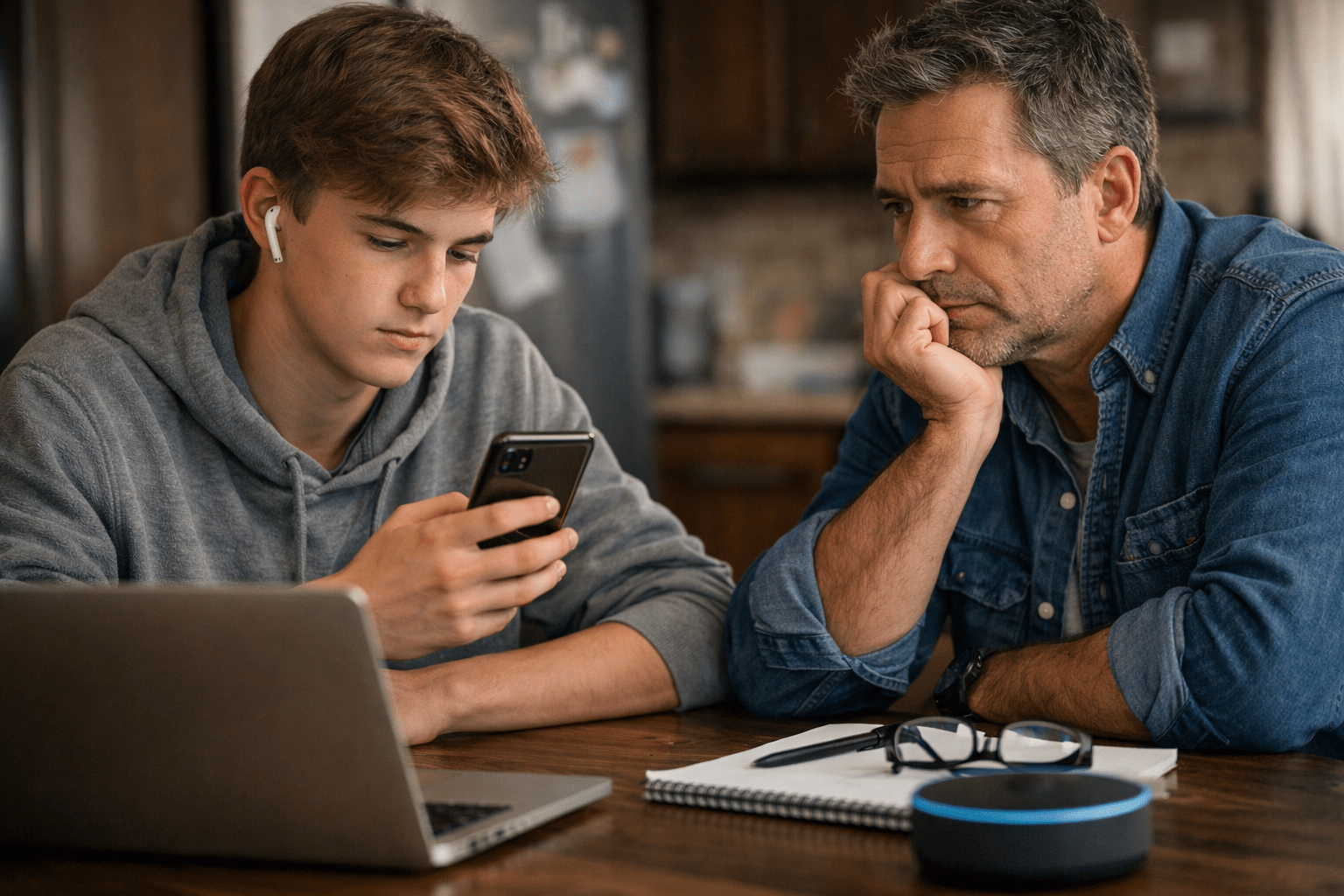
You’ve noticed something. Maybe your usually chatty teen has gone quiet. Maybe your pre-teen is suddenly anxious about everything. Maybe your young adult is struggling more than usual, and you’re not sure if this is just a phase or something that needs attention.
Is this normal? Will they grow out of it? Or is this something more?
If you’re asking these questions, you’re already paying attention. That matters.
What to Actually Watch For
According to the National Institute of Mental Health, nearly half of all adolescents (49.5%) will experience a mental disorder at some point during their teen years. Research from CAMH shows that1 in 5 Canadians experiences a mental illness. Young people aged 15 to 24 are more likely to experience mental illness and/or substance use disorders than any other age group.
These conditions are not rare. If your teen is struggling, they’re not alone. Seeking support isn’t a sign of weakness or failure—it’s healthcare, just like treating asthma or diabetes.
So what should you actually watch for? Start with something intuitive: changes that stick around and interfere with your child’s ability to do the things they need to do.
The pattern matters more than the incident. One bad day at school? Normal. Three weeks of stomach aches every morning before school? Pay attention.
Look for changes in their baseline. Your quiet kid getting quieter might mean something different from your boisterous teen having a calm week. You know your child better than anyone. Trust that knowledge.
Chances are, as parents, you will often sense something is off before specific symptoms become obvious. That gut feeling? It’s your brain processing dozens of small observations about your child’s behaviour, mood, and functioning.
What Often Shows Up
Sleep and eating patterns shift noticeably. We’re talking about changes from what’s normal for your child. The good sleeper who suddenly can’t settle in for sleep. The regular eater who stops eating or starts eating much more or less than usual. The teen who suddenly sleeps 14 hours a day or barely sleeps at all. If your teen has always been a night owl or a picky eater, that’s their normal – watch for changes from their baseline, not someone else’s.
Emotions seem overwhelming. Mood swings are part of adolescence. Watch for emotions that seem impossible to manage, persistent irritability or anger that lasts for days or weeks, frequent emotional outbursts that seem out of proportion, or your child seeming unable to regulate their feelings even with support.
Physical complaints without medical causes. Stomach aches, headaches, feeling “sick” but the doctor finds nothing wrong. The body often speaks what the mind can’t yet articulate, and physical symptoms are often how anxiety shows up in children and teens. These symptoms are real, not fake or exaggerated. Your child isn’t making it up to avoid school – their body is responding to genuine stress or anxiety.
Social withdrawal or isolation. Avoiding activities, they used to love, not wanting to see friends, struggling to maintain friendships, spending most of their time alone in their room, or dropping out of social activities completely.
Sudden shift in friend groups. All teens explore different friendships. Watch for: abruptly dropping long-standing friendships, becoming secretive about new friends or refusing to introduce them, personality changes that coincide with the new friend group, or gravitating toward peers who engage in risky behaviours like substance use, skipping school, or getting in trouble. Sometimes the friend group change is the first visible sign that something’s shifted internally.
School or work performance changes. Grades dropping, trouble concentrating, not completing work they’re capable of, increased absences, or behavioural issues that seem new or escalating.
Increased irritability, anger, or aggression. In pre-teens and teens especially, anxiety and depression often show up as irritability, short temper, or aggressive behaviour rather than sadness. Watch for excessive reactions to small things – a minor request triggers a major meltdown, or everyday frustrations lead to emotional outbursts that seem way out of proportion to the situation.
Increased or intense parental conflict. While some parent-teen conflict is normal, watch for patterns where conflict becomes frequent, intense, or seems to be about everything. Sometimes this stems from developmental mismatches – treating them like a child when they see themselves as an adult, or not understanding what the behavior is trying to communicate. Often, the surface conflict isn’t what they’re actually upset about. There are usually underlying issues at play.
Extreme academic pressure and performance stress. This is especially common when there are high expectations in the household. Watch for: obsessively studying to the point of exhaustion, refusing to come out of their room, dropping friendships to focus solely on academics, perfectionism that leads to anxiety or shutdown, or physical symptoms tied to school performance. This pressure can look like dedication on the surface but may signal unhealthy coping patterns.
Risk-taking behaviours. Experimenting with substances, reckless driving, self-harm, or other behaviours that put them at risk.
Expressions of hopelessness. Your teenager starts talking about feeling worthless, having no future, or not wanting to be here anymore. This includes indirect statements like “everyone would be better off without me” or “I wish I could just disappear.” Don’t dismiss it as teenage drama or attention-seeking. If your child expresses these thoughts, take them seriously. Talk to them, listen without judgment, and seek professional help. Contact a crisis line such as 988 for guidance on next steps – they can help you determine if you should call 911 or seek therapy support. It’s important to note that having passing suicidal thoughts is relatively common in teens, but when these thoughts become obsessive or frequent, they need immediate professional attention. Other warning signs include giving away possessions, saying goodbye to people, or sudden calmness after a period of depression.
What Normal Looks Like at Different Ages?
Ages 10-12 (Pre-teens): Increased moodiness is normal. Wanting more independence while still needing you creates contradictions. Friendship drama increases. Some self-consciousness about their changing body makes sense. Testing boundaries happens.
Ages 13-17 (Teens): Mood swings, wanting privacy, pushing boundaries, sleeping more, and increased focus on peer relationships are all normal. Friend groups naturally shift as teens explore their identity. Some conflict with parents is expected.
Ages 18-25 (Young Adults): Questioning identity, career uncertainty, relationship struggles, and adjusting to independence are all typical. Some anxiety about the future makes sense.
If you’re seeing the warning signs listed earlier in any of these age groups, that’s when typical development crosses into needing support.
When Life Gets Hard
Sometimes kids and teens need support not because something’s “wrong” with them, but because life threw something difficult their way.
Moving to a new city. Parents’ divorce. A death in the family. Loss of a significant friendship or romantic relationship. Academic pressure or failure. Bullying or social exclusion. Family conflict. Financial stress in the home (teens pick up on this more than we realize). Trauma or abuse. A pandemic that disrupted crucial developmental years.
These aren’t signs of weakness. They’re normal responses to abnormal circumstances.
Dr. Bruce Perry, a leading expert on childhood trauma and development, has shown that children and adolescents process big changes and losses differently than adults. They might seem fine initially and then struggle months later. They might express grief through anger or withdrawal. They might struggle in ways that don’t look like what you’d expect.
You don’t have to wait until your child is in crisis to seek support. Preventive care isn’t just for dental checkups.
What Therapy Offers
Some parents worry that bringing their child to therapy means admitting something is fundamentally wrong – either with their child or with them as parents. Let’s be clear: your child isn’t broken, and you’re not a bad parent. Your child is struggling with something difficult, and seeking help shows you’re a good parent who’s paying attention.
Therapy isn’t about fixing people. It’s about giving them tools, space, and support to navigate whatever they’re facing. Think of it like this: you wouldn’t wait until your child is failing every subject to get them a tutor. Therapy works the same way – it’s support, not a last resort.
Here’s what therapy actually provides:
Pre-teens and teens learn practical skills. Therapy teaches them how to identify and name feelings, develop healthy coping strategies, challenge anxious or negative thoughts, navigate complex relationships, manage stress and academic pressure, build confidence and self-worth, and communicate more effectively. Life skills they’ll use forever.
A safe, confidential space. Sometimes young people need somewhere to talk without worrying about upsetting their parents or being judged by peers. Therapy provides that neutral ground where they can be completely honest.
Better self-understanding. Adolescence and young adulthood are times of significant identity development. Therapy can help young people understand their emotions, motivations, and patterns in ways that promote healthy development.
Addresses specific challenges. Whether they’re dealing with anxiety, depression, trauma, grief, relationship issues, academic stress, substance use, or identity questions, therapy provides evidence-based approaches tailored to their specific needs.
Prevention. Research shows that early intervention for mental health challenges significantly reduces the risk of ongoing difficulties in adulthood.
Our children and youth therapists, Lauren, Nada and Karoline, specialize in creating this safe, supportive environment where young people can be themselves and develop the skills they need to thrive.
Talking to Your Child About Therapy
Important: If your child shares thoughts of self-harm or suicide with you, this requires immediate attention.
First, stay calm and listen without judgment. Let them know you hear them and you’re going to help them get support.
Then, contact a crisis line such as 988 (suicide crisis helpline) or Kids Help Phone at 1-800-668-6868 (text CONNECT to 686868). These crisis counsellors can help you assess the situation and determine the appropriate next steps.
Call 911 only if you believe your child is in immediate danger and will not be safe.
Many teens experience thoughts of self-harm or suicide, and while these are serious warning signs that need professional support, calling 911 for thoughts without a plan may result in hospital admission and could make your teen less likely to share their feelings with you in the future.
The guidance below is for conversations about ongoing therapeutic support.
Many parents find it difficult to bring up therapy with their child. How do you start this conversation without making them feel like something’s wrong with them?
Keep it simple and honest. Match your language to their age and maturity level.
For pre-teens (10-12): “I’ve noticed you’ve been having a tough time with [a specific thing]. I think it might help to talk to someone who works with kids dealing with these kinds of feelings. Kind of like having a coach, but for emotions and problems. Many kids your age see someone like this. What do you think?”
For teens (13-17): “I care about you, and I’ve noticed [specific observations]. I think talking to a therapist might help. There are therapists who work with teens dealing with similar challenges. What you talk about is completely private between you and the therapist. You don’t have to tell me anything. Would you be open to trying it?”
For young adults (18+): “I’ve noticed you seem to be struggling with [specific concern]. Have you thought about talking to someone? A therapist could help you work through this. I’m happy to help you find someone if you like, or you can look on your own. Either way, I’m here to support you.”
What helps:
- Normalize it. Many young people see therapists. It’s a sign of strength, not weakness.
- Be honest about why you think it might help, but don’t dramatize it.
- Reassure them therapy is confidential (within legal limits).
- Emphasize that it’s their space to talk about what matters to them.
- Let them have some input in choosing a therapist if possible.
- Answer their questions honestly.
What doesn’t help:
- Making it sound like punishment
- Calling it “fixing” them
- Minimizing their feelings (“You have nothing to worry about!”)
- Forcing it without any explanation or discussion
- Threatening consequences if they don’t go
- Ignoring the behaviour and hoping it goes away
Many teens and young adults have shared that they wished their parents had said something when they were struggling. Talking about your concerns is almost always better than saying nothing. Even an imperfect conversation shows you care and are paying attention.
Some teens will resist initially. That’s okay. Let them know you hear their concerns, and you’re still moving forward because you care about their well-being. For young adults, you can offer support but ultimately respect their autonomy in the decision.
Your Next Steps
Trust yourself. If your gut says something’s off, listen to that. You can always consult a therapist and decide therapy isn’t needed right now. Ignoring persistent concerns doesn’t make them go away. We offer complimentary 15-minute consultations.
Start with your family doctor if you’re unsure. They can rule out medical causes and provide a referral.
Look for therapists who specialize in adolescents and young adults. Not all therapists work effectively with this age group. Find someone trained in adolescent development and evidence-based approaches for teens and young adults.
Don’t wait for a crisis. Earlier support often means easier progress.
Consider an initial consultation. Many therapists offer a first meeting to assess whether therapy would be helpful. At Cornerstone, a 15-minute complimentary call with our team can help you determine if therapy is the right fit for your child or teen right now.
Therapy works. Research shows substantial evidence for the effectiveness of psychotherapy with children and adolescents, particularly when therapists use evidence-based approaches like Cognitive-Behavioural Therapy (CBT), Interpersonal Therapy, and other proven methods. These aren’t experimental treatments – they’re approaches with solid research backing their effectiveness for anxiety, depression, behavioural challenges, trauma, and life transitions.
The Bottom Line
Your child doesn’t need to be in crisis to benefit from therapy. They don’t need a diagnosis.
If your teen is avoiding school because of anxiety, if friendship drama is consuming their thoughts, if they’re withdrawing from activities they used to love, if academic pressure is overwhelming them, if grief is hitting them harder than expected, or if you simply sense something is off – those are all reasons to reach out.
Early support isn’t about preventing failure. It’s about giving your child tools when they need them most.
Seeking help for your child isn’t an admission of failure as a parent. It’s an act of love. It’s saying, “I see you struggling, and I’m going to make sure you get the support you need.”
That’s good parenting.
Book a free 15-minute call with Karoline, Lauren or Nada to discuss your concerns. Karoline and Nada offer therapy in Arabic and English. They can help you determine whether therapy is the right fit for your child right now and answer any questions you have. Our youth specialists work with pre-teens, teens, and young adults using evidence-based approaches in a warm, safe environment.
Call us at 905.214.7363 or email [email protected].
Sometimes the bravest thing a parent can do is ask for help.